World Health Organization (WHO) removes Barbados as a country threatened by the Zika virus
Effective from Friday 19th October 2018, WHO has removed Barbados as a Zika infected country. New data from CARPHA showed that the Caribbean region had shown no signs of Zika virus in over 12 months and therefore poses little or no threat to residents or visitors.
The outbreak of Zika virus in early 2016 was of great concern to us here at the clinic and the world spotlight was on countries where Zika virus had been reported. Our medical team worked tirelessly to ensure we had the latest up to date information for our patients and that patients undergoing IVF during this time were not put at any adverse risk.
The Zika virus was transmitted via a mosquito bite, which can be prevalent during the rainy season, so we are delighted that Barbados is no longer considered to be a country where you may get infected with Zika virus.
We do still advise our patients to take the necessary precautions to avoid mosquito bites using repellants during dawn and dusk and to reapply frequently. Your well-being during your stay in Barbados is paramount and key to successful IVF treatment with us.
For more information on the CARPHA report that led to WHO making the decision to remove Barbados from the list of Zika infected countries, please click here.
Learn More
Polycystic Ovarian Syndrome (PCOS): an infertility issue that is little understood.
Polycystic Ovarian Syndrome (PCOS): an infertility issue that is little understood.
Polycystic Ovarian Syndrome (PCOS) is one of the primary causes of a woman’s infertility. Between the age of 20 to 40, PCOS affects somewhere between 5% to 10% of women. This makes it the most widespread reproductive syndrome for this age group of women.
Since PCOS cannot be diagnosed with one test alone and symptoms vary from patient to patient, PCOS is known as the ‘Silent Killer’ and can result in misdiagnosis, with 30% of women never being diagnosed.
What Exactly is PCOS?
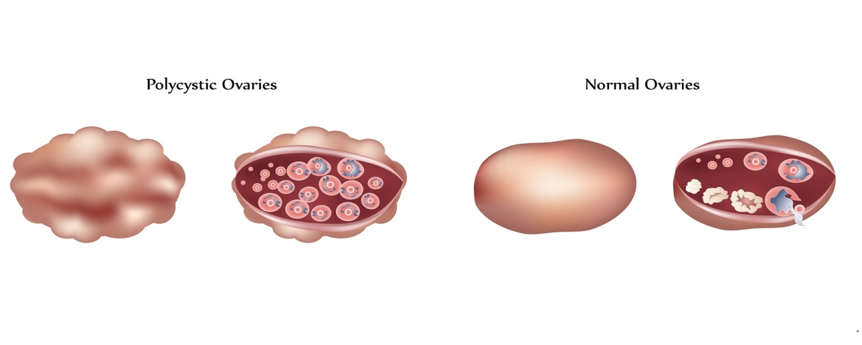
PCOS is a complex, heterogeneous disorder of uncertain etiology, although recurrence in the same family is often observed supporting a genetic origin.
According to the so-called Rotterdam criteria, a woman with any two of the following conditions may have the condition:
■ Symptoms of elevated levels of androgens, or male sex hormones, which can include acne, excessive hair and sometimes male-pattern hair loss.
■ Irregular menses, with prolonged periods between cycles.
■ Polycystic ovaries, as seen on an ultrasound.
Regrettably, PCOS is one of those reproductive syndromes that often goes undiagnosed.
Early diagnosis of PCOS is important to avoid long term complications such as increased risk for developing insulin resistance, type 2 diabetes, high cholesterol, high blood pressure, heart disease and endometrial cancer.
Treatment of PCOS
Patients with PCOS who don’t wish to conceive.
Patients with PCOS who don’t want to conceive should be treated to control immediate symptoms and to avoid long term complications.
Consuming a healthy diet and regular exercise, controlling weight, glucose and insulin levels is effective and recommended as first approach.
In many cases, birth control is prescribed in order to decrease hormone levels, normalize the menstrual cycle and minimize acne appearances.
Due to the fact that insulin-resistance is common in women who have been diagnosed with PCOS, medications such as metformin are typically prescribed as well affecting how insulin controls glucose and reducing testosterone.
Metformin improves menstrual cycling, slows hair growth, reduces body mass, reduces cholesterol levels and improves ovulation induction response. Surgery called ovarian drilling is one option for PCOS, although it is only recommended as a last resort and in most of the cases the effects are only temporary.
PCOS and Infertility – Patients with PCOS who are trying to conceive.
More than 95% of women with PCOS do not ovulate regularly, have irregular menstrual cycles and struggle to conceive naturally. With Inanovulatory cycles, the ovarian follicles fail to mature and release eggs. Treatment to promote the recruitment and release of the egg is required (ovulation induction).
PCOS requires management to conceive in most of the cases. Optimal management means we rule out coexisting causes i.e. tubal assessment and semen analysis, ovulation induction strategies are closely monitored on a time line.
Ovulation induction programs are very successful in PCOS:
* 80% of patients achieve the goal of follicular development and egg maturation with oral agents such as clomid.
* 15 % of patients needs injectable agents
* Only 5% of PCOS cases need IVF, and are usually successful!
Reach out to us if you need to discuss IVF help if you suffer from PCOS.
– Dr Corona


Managing PCOS
Managing PCOS
To learn more simply complete the form below and a copy of the presentation will be emailed to you to watch in the comfort and privacy of your own home:
GET IN TOUCH
Get in touch to sign up for a free, no obligation phone consultation with our IVF Specialist Physicians.

IVF Monitoring: What is it?
‘Monitoring’ is a general name for the activities of ultrasound and/or bloodwork testing, to evaluate how a woman is responding to her stimulation treatment. The results of the ultrasound and/or bloodwork are reviewed by the physician, and further instructions for continued treatment are shared by the patient’s nurse.
This is a general explanation of the routine IVF monitoring which all patients undergo during their cycle. But it is not so simple. Often we receive questions like: “what is the best monitoring?”, “should it be done daily?”, “how many scans are needed?”, “Is blood test always necessary”, and many, many, many more!
With this blog I am going to try answering to some of these questions in a very simple way.
Let’s go step by step.
Methods of monitoring
There are basically 2 tools available for monitoring: ultrasound and blood test.
The ultrasound technique used mostly is the 2D trans-vaginal scan. 3D technology can sometimes be added as well as power color Doppler to evaluate vascularization. Trans-abdominal ultrasound (TVUS) is used less but it can be necessary in some cases i.e. when the ovaries are very high in the abdomen.

Hormonal blood testing includes E2 (Estradiol) levels, P (progesterone) and LH (luteinizing hormone). The E2 is produced inside the developing follicle. The blood E2 level helps to the correlate growth of the follicle with maturation of the egg. The blood LH level indicates when a woman is about to ovulate. This helps with the timing of ‘timed intercourse’ and IUI treatment cycles, it is not used in IVF cycles. Progesterone normally rises in serum after ovulation and trigger endometrial maturation necessary for implantation (uterine receptivity). Testing progesterone can be therefore very useful for instance when a premature ovulation of one of the follicles is suspected or in a long stimulation with risk of premature LH surge.
Combining the methods of monitoring
We have established what are the methods available but how shall we use them? Let`s use science and evidence based medicine to help us answer this.
The first controversial question that we tried to answer was whether TVUS and E2 should be combined. Several studies were done and results showed that E2 measurements are unnecessary, time consuming, expensive, create anxiety for the couple and are inconvenient for the women (Rainhorn 1987; howard 1988; Tan 1992). Minimal monitoring (only as less as possible TVUS) showed to have no adverse effect on treatment outcomes and it does not increase the risk of OHSS (Abdalla 1989; Tan 1994; Roest 1995). Based on these results, several IVF programs have abandoned the use of hormonal essay completely without recording any significant change in their outcomes (Kemeter 1989; Vlaisavljevic 1992; Tan 1994).
Many more studies have been conducted after these, investigating different specific outcome of the stimulation cycle like number of oocytes, clinical pregnancy rate and OHSS rate. A study done in 2014 (Gynecol Endocrinol. 2014 Sep;30(9):649-52) clearly showed that adding serum estradiol measurements to ultrasound monitoring does not change the yield of mature oocytes in IVF/ICSI.
Cochrane is a global independent network of researchers and professionals formed to organize medical research findings collecting only high-quality independent evidence to inform healthcare decision-making. In 2008 and then updated in 2014, Cochrane published a systematic review collecting and analyzing together the most reliable and relevant articles on this topic conducted in the UK, France, Spain, Israel and the US with the following results: “This review update found no evidence from randomised trials to suggest that combined monitoring by TVUS and serum estradiol is more efficacious than monitoring by TVUS alone with regard to clinical pregnancy rates and the incidence of OHSS. The number of oocytes retrieved appeared similar for both monitoring protocols. The data suggest that both these monitoring methods are safe and reliable”.
So, what is the best monitoring?
I think the answer to this is personalized monitoring.
We at BFC do not have a “one-size-fits-all” treatment plan for IVF and therefore we do not have inflexible monitoring protocols. We strongly believe in evidence based medicine so we do not practice standard daily combined TVUS and blood test as there is no clinical reason why this would increase your chances of success, nevertheless we know every woman who undergoes IVF treatment is unique. Each couple presenting to an IVF clinic has an individual infertility cause and medical and fertility history. It is essential to customize a unique therapeutic scheme for each couple, offering the opportunity to be flexible during ovarian stimulation. During treatment, your personal physician is monitoring your results, constantly communicating with you and the team about the next best step for your treatment, like asking for an extra ultrasound or blood test, adjusting your medication dosage for your optimal response, and determining the best day for your egg retrieval, taking always into account your personal history.
This is a prerequisite, for achieving the best outcome and defines the success or failure of an IVF treatment cycle.
– Dr Corona


BFC are coming to Trinidad to meet you!
The team from Barbados Fertility Centre are coming to Trinidad to answer your fertility questions and concerns on how to achieve maximum IVF success.
The free seminar will be held on Sat Sept 29th from 9am – 1pm at Centre of Excellence, 17A Macoya Rd, Tunapuna, Trinidad. Our leading IVF specialists, Dr. Juliet Skinner and Dr. Roberta Corona will be presenting on how you can achieve successful IVF in Barbados. You will have the opportunity to ask questions and meet previous patients who made the decision to have IVF treatment with us.
Refreshments will be provided and time has been allocated for questions and answers.
It is free of charge to attend but you do need to register for a place as seating is limited by going to http://www.meetbfc.com
Learn More

